Home
A Broad Introduction
Allergy Concepts
Food Issues
Asthma
Rhinitis & Hay Fever
Eczema
Children & Infants
Allergy to Animals
Finding Answers



|
 |
|
Shortcuts to
sections on this page |
|
|
|
|
|
Professional Status
There are so few allergists in
this country that many dubious practitioners have attempted to
satisfy this unmet need. For this reason it is essential to
establish my medical professional status by a brief account of my
career.
I qualified as MB ChB at Edinburgh University in 1939, and served in
the Royal Army Medical Corps throughout the war, mainly in India,
until 1946. Post-graduate studies in Edinburgh led to the award of
the degree of MD with Commendation in 1950 for my thesis on
"Adaptation and Adaptive Dysfunction". In 1949 I became a Member of
the Royal College of Physicians of Edinburgh, and was elected a
Fellow of the College in 1965.
After experience in the
Professorial Unit at Dundee Medical School under Professor Sir Ian
Hill, and in the Dundee Chest Clinic, I was appointed Consultant
Chest Physician South Derbyshire In 1953, and later Allergist to the
Derwent Hospital, Derby Chest Clinic, and the Derby Children's
Hospital.
So many practitioners in the Derbyshire/Nottingham area who knew me
well have retired, and younger colleagues are unaware that I am
still in active consulting practice. It may be helpful when
requesting a referral that your doctor should be made aware that,
firstly, I
am one of the very few GMC Registered Specialists for Allergy and
Respiratory Medicine, secondly, of this website and, thirdly, of my
international reputation
 Allergy Research Allergy Research
I carried out many research
projects in allergy and in aerobiology during the last 30 years. I
also founded that Midlands Asthma and Allergy Research Association
in 1968 to support allergy research in the Midlands and organised
five International Symposia on Clinical Allergy at Nottingham
University.
In 1993 I was awarded the Charles Blackley Lectureship by the
British Society for Allergy and Clinical Immunology, in 1999 the
William Frankland Medal for services to Clinical Allergy, and in
2004 I received an Honorary Doctorate from Derby University.
I belong to the British, American, and European Societies for
Allergy and Clinical Immunology and still present new research at
annual meetings. In 2006 I was elected as an International Fellow
of the American Academy of Allergy Asthma and Immunology, being only
the tenth British doctor thus honoured by the most prestigious
Allergy Association in the world. I continue in active clinical
practice not only because I enjoy seeing patients and solving their
problems, but because there are so few allergy specialists. It is a
paradox that while Britain has the highest incidence of allergic
disease in the world, it also has the most inadequate allergy
service.
My objective has always been to find the cause rather than suppress
the symptoms with drugs which may have side-effects and can never
cure. For example antibiotics will cure an infection completely, but
drugs for allergies only suppress the symptoms of asthma, rhinitis,
or eczema. To rely on drugs alone without at least trying to find
the cause seems an inadequate approach to allergic problems.

 Major Researches - A
Brief Outline Major Researches - A
Brief Outline
In 1958 I demonstrated that if
many eosinophil cells, which are typical of allergy, were present in
the sputum from patients with asthma they would be greatly helped by
oral steroid tablets. When eosinophil cells were absent patients did
not improve when given steroids, and the correct diagnosis was
chronic bronchitis. The publication of this work in the Lancet by
only one researcher, not double-blind, and with only one table of
results and no statistics, would never have had a hope of being
accepted for publication today, but has proved to be a really
important observation because it enabled selection of the patients
who would benefit from oral steroids from those who would not, and
is used widely in important research to this very day.
|
|
|
 |
|
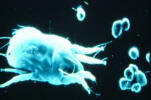
Mast Cell in nasal smear
|
Eosinophils stained red in
sputum |
Macrophages in bronchitic
sputum
|
Following this development I
soon had hundreds of very happy asthmatic patients taking steroid
tablets. Unfortunately oral steroids also have long-term
side-effects, and in my opinion should be regarded as a chemical
crutch to control the allergy while a search is made for the cause.
In my contribution to a Symposium on Airways Obstruction at the
Royal Festival Hall in 1969 I stated "Steroids pave the primrose
path of therapeutic dalliance, leading only to a mirage of apparent
health and well-being". Perhaps this was an extreme view, but
sometimes appropriate.
Because the presence of many eosinophil cells usually indicates that
an allergic reaction is taking place I became deeply involved in
allergy research directed at finding the innumerable causes of
asthma, rather than relying on indefinite suppression of symptoms
with drugs. It seemed obvious that if the cause or causes of the
asthma could be found and avoided there would some possibility of
getting patients off steroid treatment, or at least controlling the
asthma with a smaller dosage of steroid.
If the cause was found to be unavoidable desensitising injections
could then be given in the patients no longer reacted to the
allergen, and then steroids could be stopped altogether or the
dosage reduced considerably. Success with these methods,
particularly in asthma, encouraged my interest in finding the causes
of other allergic diseases such as allergic rhinitis, hay fever,
eczema, anaphylaxis, and food allergies, often involving other
medical specialties.

 The Rescue of Becotide,
the first Inhaled Steroid The Rescue of Becotide,
the first Inhaled Steroid
The ability to select the
allergic patients most likely to respond to steroids by sputum
examination, was the reason
why I was given the opportunity to carry out a clinical trial of the
very first inhaled steroid, Beclomethasone Dipropionate, (later
named Becotide) beginning in July 1970.
 This clinical trial was of
crucial importance because trials in Edinburgh from 1968 had failed
to show any benefit, probably because cases of chronic bronchitis
were selected. The makers, Allen & Hanburys, were just about to
discard Becotide as a useless drug on the basis of these poor
results, but their Medical Director did not agree because he had
heard me lecture about selecting responders to steroids by sputum
cytology. He wrote to me stating that his last act before taking up
a new appointment was to ask me to try the steroid aerosol because
he was so sure that it would be effective. I then commenced a
clinical trial selecting only patients with eosinophils, and my
results, monitored for the very first time by giving peak flow
meters to every single patient, were so impressive that after six
months the manufacturers wrote stating that they had decided "to
give the steroid aerosol another chance". This clinical trial was of
crucial importance because trials in Edinburgh from 1968 had failed
to show any benefit, probably because cases of chronic bronchitis
were selected. The makers, Allen & Hanburys, were just about to
discard Becotide as a useless drug on the basis of these poor
results, but their Medical Director did not agree because he had
heard me lecture about selecting responders to steroids by sputum
cytology. He wrote to me stating that his last act before taking up
a new appointment was to ask me to try the steroid aerosol because
he was so sure that it would be effective. I then commenced a
clinical trial selecting only patients with eosinophils, and my
results, monitored for the very first time by giving peak flow
meters to every single patient, were so impressive that after six
months the manufacturers wrote stating that they had decided "to
give the steroid aerosol another chance".
Thus the first steroid aerosol was rescued from the dustbin and a
new era in the treatment of asthma began. I was the first in the
world to publish reports on the remarkable effectiveness of inhaled
steroids in both adults and children in the British Medical Journal
in 1971 and 1972.
This research would have been very difficult to carry out under the
strictures which govern clinical trials today, and would be
unacceptable for publication because this was not a double blind
study where neither doctors nor patients know who is receiving
active drug or placebo. By using daily peak flow readings In this
trial the improvements were so obvious that the results were
accepted without question.
This treatment was soon used all over the
world because inhaled steroid aerosols act directly on the bronchial
tubes and control asthma without side-effects, while oral steroids
circulate in the bloodstream, causing side-effects as well as
remarkable benefits, depending on the dose. One of the most
important findings was that many patients dependent on oral steroids
could stop the tablets and be controlled by the inhaled steroid
instead without side-effects.
 Inhaled steroids are now acknowledged to be the most important
development in the treatment of asthma in the last thirty years, so
I am very proud that the trials in Derby were the first to show
their effectiveness. Very few asthmatics need oral steroids today
except in emergency, and total dependence on oral steroids is
unusual. Inhaled steroids are now acknowledged to be the most important
development in the treatment of asthma in the last thirty years, so
I am very proud that the trials in Derby were the first to show
their effectiveness. Very few asthmatics need oral steroids today
except in emergency, and total dependence on oral steroids is
unusual.
Many effective inhaled steroid compounds were developed over the
following years, but recent improvements in the propellant gas used
in the aerosol have resulted in the particles of the aerosol being
so small that they penetrate to the very smallest bronchial tubes,
enabling the whole bronchial tree to be treated for the very first
time. This may be very important for chronic asthmatic children who
have to take inhaled steroids for life.
When I arrived in Derby in
1953 tuberculosis was a major problem, Chest Clinics looked after
the whole family from cradle to grave, and patients were followed up
from infancy onwards. After tuberculosis was controlled allergy
became my major interest and, as the old TB clinic organization
allowed me to treat children, I continued to do so, and to observe
how allergy or intolerance to milk and other foods could be
inherited.
This unique personal experience would be impossible today because
the development of organ specialties has created barriers to the
generalised approach which, in my opinion, is essential for the
recognition of the diverse clinical problems caused by faulty
adaptation to the environment, of which the commonest manifestation
is allergy.

 Recent Researches and
Publications Recent Researches and
Publications
During my time within the
National Health Service I was fortunate to have freedom to follow my
research interests and develop a very active research unit. I am
certain that these achievements would have been quite impossible
under the restrictive bureaucracy imposed today. Fortunately, the
development of the World Wide Web gives me a wonderful opportunity
to publish these researches and experience for all to share.
 I continue to publish new
research, and recently was involved in a report in the Lancet where
I personally diagnosed the first case of anaphylaxis in the UK to be
caused by lupin flour. This is a hidden menace because the commonest
dangerous food allergy is to peanuts, and many peanut allergics are
also sensitive to lupin, which did not have to be declared on the
label until recently. I continue to publish new
research, and recently was involved in a report in the Lancet where
I personally diagnosed the first case of anaphylaxis in the UK to be
caused by lupin flour. This is a hidden menace because the commonest
dangerous food allergy is to peanuts, and many peanut allergics are
also sensitive to lupin, which did not have to be declared on the
label until recently.
In recent years I have seen an increasingly wide range of illnesses
not usually recognized as due to allergy or intolerance, especially
IBS and similar gut disorders. Dietary manipulation has been very
helpful in many cases.
In 2007 The Annals of Allergy and Clinical Immunology, a prestigious
American medical Journal, published my long letter to the editor
suggesting that very very gradual reintroduction of a food such as
peanut in microscopic doses, increased carefully until tolerated
without reactions, might be a better approach than strict avoidance
with the constant fear of anaphylaxis from eating a trace of peanut.
Another letter relating the story of how Becotide, the most
important advance in treatment in the last 35 years, was nearly
discarded as useless was also published in this journal in 2007
 Specialised Facilities for
Investigation and Treatment Specialised Facilities for
Investigation and Treatment
I see patients of all ages,
especially children, including infants with feeding problems. At my
consulting rooms I have developed specialised facilities for the
out-patient investigation of all sorts of allergies. These include a
very wide range of skin tests, patch tests if necessary, electronic
lung function testing, oximetry, and typmpanometry for investigating
glue ears etc.
 Microscopical examination of the cells in the sputum or nasal
discharge, and of samples of house-dust when required, is carried
out on the spot, and relevant blood tests are available when
required. Microscopical examination of the cells in the sputum or nasal
discharge, and of samples of house-dust when required, is carried
out on the spot, and relevant blood tests are available when
required.
A completely unique investigation is making special
extracts from samples of the patient's own house dust or the hair of
their pets. This is make a skin test from the patientís own
environmental dust to
establish the importance of the patient's own home environment. This
innovative and logical method of investigation can pinpoint the
source of allergy in the home, assess its importance, and indicate
what action should be taken.
Allergy problems are often complicated and require much time and
expertise to sort out, so I find it best to regard the sufferer as a
partner in the investigation rather than as a patient.
The objectives of an allergy consultation are to identify the cause
of the problem, assess its severity and impact on the quality of
life, and to ensure that the most up-to-date treatments are being
used in the most effective manner.
Patients always receive a copy of my report, as well the family
doctor, because this prevents misunderstandings, encourages
compliance with my suggestions, reassures the patient, and provides
a back-up against loss of medical records.
|